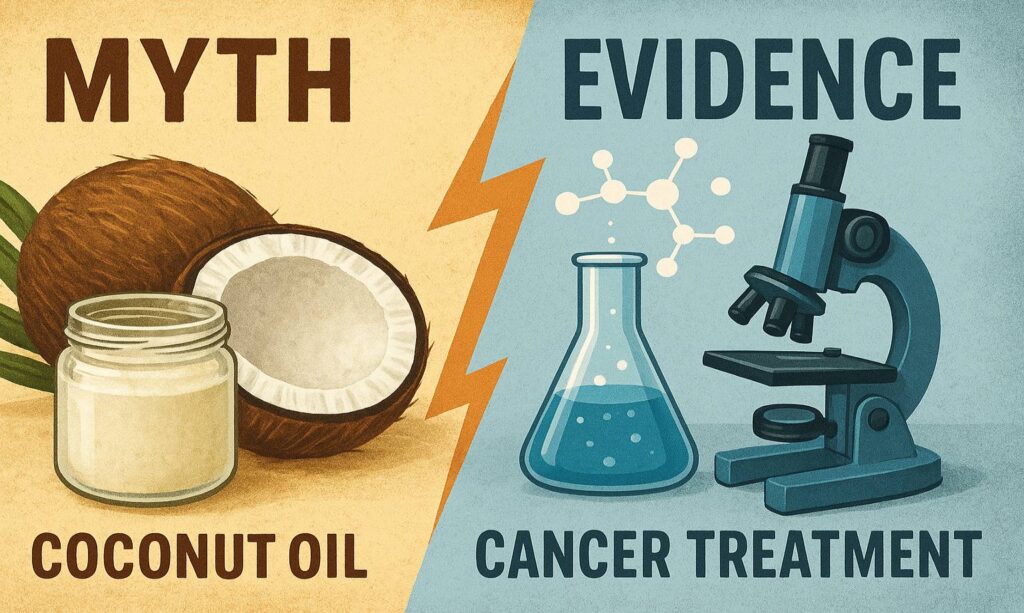
The claim that coconut—whether oil, water, or kernel—treats cancer is compelling but unsupported by clinical evidence; lab and animal findings do not translate into proven human therapies, and substituting coconut for standard care can be dangerous. This article uses a skeptical, evidence-first structure to separate petri-dish promise from patient-level reality while offering practical guidance and a concise table comparing claims vs. evidence.
Executive Summary
- Coconut compounds show anticancer activity in cells and some animal models, but no human clinical trials demonstrate treatment or cure.
- Coconut water supports hydration; coconut oil is a saturated fat with cardiovascular trade-offs; neither replaces surgery, chemotherapy, radiotherapy, or immunotherapy.
- If coconut-derived molecules ever help in oncology, it will likely be through engineered formulations tested in trials—not kitchen remedies.
Why This Claim Persists
- “Natural” and familiar foods feel safer and more approachable than pharmaceuticals.
- Early-stage studies are often misread as clinical proof, amplified by online echo chambers.
What Counts as Evidence
- In vitro studies test cells in dishes.
- Animal models explore mechanisms and dosing.
- Human evidence requires controlled clinical trials that demonstrate safety and efficacy.
Preclinical Findings: What the Lab and Animals Show
In Vitro (Cell Studies)
- Lauric acid and virgin coconut oil (VCO) have shown apoptosis induction, oxidative stress increases, and cell-cycle effects in certain cancer cell lines.
- Nanoemulsion or delivery-system studies can enhance drug effects in dishes, but these are not equivalent to eating coconut oil.
Animal Models
- Extracts from coconut kernel and related lipids have reduced tumor markers or lesion formation in select rodent models.
- Doses, formulations, and tumor biology differ from humans, and results often fail to replicate in clinical settings.
The Human Evidence Gap
No Proven Treatment Effect
- There are no high-quality randomized trials showing coconut oil, kernel extract, or coconut water treat or cure cancer in humans.
- Major oncology guidance emphasizes comprehensive nutrition to tolerate therapy—not coconut as therapy.
Nutrition vs. Therapy
- Coconut water can aid hydration; coconut oil is calorie-dense and high in saturated fat; neither has demonstrated anticancer efficacy in human trials.
- Replacing or delaying evidence-based treatments for coconut products risks worse outcomes.
Safety, Trade-offs, and Realistic Roles
Cardiometabolic Considerations
- Coconut oil’s saturated fat can worsen lipid profiles; survivors and patients on cardiotoxic regimens should weigh cardiovascular risks.
- Unsaturated fats (e.g., olive, canola) are generally preferred within oncology nutrition guidance.
Adjunct Hypotheses (Unproven)
- Some rodent and mechanistic data suggest potential mitigation of treatment toxicity or pathway modulation; this remains hypothesis-generating.
- Pharmacokinetics, bioavailability, and tumor microenvironment constraints mean dietary intake is unlikely to reach therapeutic concentrations.
Practical Guidance
For Patients and Caregivers
- Do not substitute coconut products for prescribed treatments; discuss any supplements with the oncology team.
- Culinary use of coconut in moderate amounts can fit a balanced diet; prioritize total protein, calories, and unsaturated fats for treatment tolerance.
- Evaluate claims by asking: Is there a peer-reviewed human trial? What outcomes improved? Are risks addressed?
For Clinicians
- Acknowledge interest in natural approaches while clarifying evidence tiers.
- Screen for high-dose coconut oil use in patients with dyslipidemia or cardiac risk.
- Guide toward reliable nutrition resources and, when appropriate, registered dietitians specialized in oncology.
Comparative Table: Claims vs. Evidence
| Coconut Product / Claim | What’s Claimed | What Preclinical Shows | Human Evidence | Key Risks / Considerations |
|---|---|---|---|---|
| Coconut oil treats cancer | Kills cancer cells, shrinks tumors | Apoptosis and antiproliferative effects in select cell lines; signals in some rodent models | No randomized trials showing treatment benefit | High saturated fat; potential lipid profile worsening; treatment delay risk |
| Lauric acid is anticancer | Targeted cancer killing | Mechanistic apoptosis/ROS/cell-cycle effects; delivery-system promise in vitro | No proven clinical efficacy as a standalone or supplement | Unknown effective dosing in humans; bioavailability limits |
| Coconut water cures cancer | Natural cure via hydration/electrolytes | Not applicable | No evidence of anticancer effect; hydration support only | Treatment substitution risk; sugar content concerns in some patients |
| Coconut as chemo adjunct | Reduces toxicity, boosts drugs | Rodent signals of toxicity modulation; nanoemulsion delivery synergy in vitro | No validated clinical benefit | Requires controlled trials; interactions unknown |
Bottom Line
- Coconut’s lab signals are real but preliminary; human therapy claims are not supported.
- Use coconut products as food, not medicine; keep intake moderate and within a heart-healthy plan.
- Real oncology advances from coconut-like compounds will come, if at all, via rigorous trials and engineered formulations.